The Role of Hormones in Weight Management and Appetite Regulation
Key Takeaways
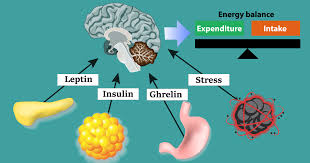
- Hormones play a major role in appetite, metabolism, and weight control.
- Imbalances in leptin, ghrelin, insulin, and cortisol can hinder weight loss.
- Gut hormones influence fullness and respond to diet choices, especially protein.
- Diet, exercise, sleep, and stress management help support hormonal balance.
Introduction
Hormones are powerful regulators of appetite and body weight, influencing nearly every aspect of how our bodies respond to food and energy balance. By understanding the science behind these chemical messengers, individuals can better navigate the challenges of weight control. For those seeking professional guidance, Options Medical Weight Loss offers personalized support that incorporates the latest research on hormone-driven weight management.
The way hormones interact with eating behaviors and metabolism explains why weight gain or loss can be more complex than simply counting calories. Factors like chronic stress, sleep patterns, and even gut health all play essential roles in how our bodies signal hunger and satiety. These insights can help create more successful and sustainable strategies for achieving and maintaining a healthy weight.
Key Hormones Involved in Appetite Regulation
Leptin: The Satiety Hormone
Leptin is produced primarily by fat cells and communicates directly with the brain to help regulate hunger. When fat stores are sufficient, leptin levels rise, signaling the brain to reduce food intake. However, this process may become disrupted in people with obesity, who often develop leptin resistance. As a result, the brain stops responding efficiently to leptin’s signals, promoting increased food consumption and further weight gain. Experiencing difficulty feeling full can often be traced to disturbances in this hormonal pathway.
Ghrelin: The Hunger Hormone
Often called the ‘hunger hormone,’ ghrelin is released mainly from the stomach, especially when it is empty. Ghrelin travels to the brain, stimulating appetite and triggering the sensation of hunger before meals. Once food is consumed, ghrelin levels fall. Interestingly, individuals with excess weight commonly display higher circulating levels of ghrelin after diets, making weight maintenance particularly challenging. This hormonal feedback loop is why long-term weight-loss programs must address changes in ghrelin, not just caloric intake.
Insulin: The Blood Sugar Regulator
Insulin, secreted by the pancreas, is vital for moving glucose from the bloodstream into cells for energy. Chronically elevated insulin levels, often a consequence of insulin resistance, are associated with the onset of type 2 diabetes and increased body fat storage. This can make losing weight more difficult and increase the risk of developing metabolic diseases. According to the Centers for Disease Control and Prevention, managing blood sugar and insulin through diet and exercise is a cornerstone of healthy weight management.
Cortisol: The Stress Hormone
Elevated cortisol levels, often a result of chronic stress or inadequate sleep, can significantly increase appetite. This hormone is known for encouraging cravings for calorie-dense, sugary, or fatty foods, which can eventually lead to unwanted weight gain. Over time, cortisol’s impact on eating behaviors can make sustained weight loss more difficult and underscore the importance of stress management for overall metabolic health.
Gut Hormones and Their Impact on Appetite
Cholecystokinin (CCK)
CCK is released by the small intestine during meals and is a powerful satiety-promoting hormone. It slows gastric emptying and communicates with the brain to encourage meal termination. Research has shown that in people with obesity, the response to CCK may be blunted, reducing its ability to naturally curb food intake. Greater awareness of gut hormone function can therefore aid in tailoring diet plans to specific needs.
Peptide YY (PYY)
Peptide YY is another significant gut hormone that helps suppress appetite after meals. Higher protein diets have been found to increase PYY levels, which might explain why these diets can be particularly effective for weight loss. Conversely, individuals with obesity may have lower baseline PYY, contributing to increased appetite and challenges in calorie control.
Strategies to Balance Hormonal Influence on Weight
- Balanced Diet: Eating a range of wholesome foods, including plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats, helps modulate the function of critical hormones such as insulin and ghrelin. Nutrient-dense meals prevent sharp blood sugar spikes and promote steady energy levels.
- Regular Exercise: Incorporating physical activity into your routine improves insulin sensitivity and helps to regulate cortisol levels, making it easier to maintain a healthy weight. Activities such as walking, resistance training, and aerobic exercise each contribute unique metabolic benefits.
- Adequate Sleep: Aiming for seven to nine hours of quality sleep each night supports healthy levels of both leptin and ghrelin. Consistent restful sleep also reduces the risk of late-night snacking triggered by hormonal imbalances.
- Stress Management: Practicing mindfulness, meditation, or yoga can lower cortisol levels, reducing the risk of stress-related weight gain and helping maintain better hormonal balance throughout the day.
Final Thoughts
Hormones are at the heart of weight management and appetite regulation, affecting how the body senses hunger and stores energy. A thorough understanding of how these chemical signals operate enables the tailoring of diet, exercise, and lifestyle interventions for long-term success. Leveraging insights into hormone function can transform weight loss journeys and improve overall well-being.